

HealthCare Quality | Follow the money
Which stakeholder has the most influence on healthcare spend and trends? Why?
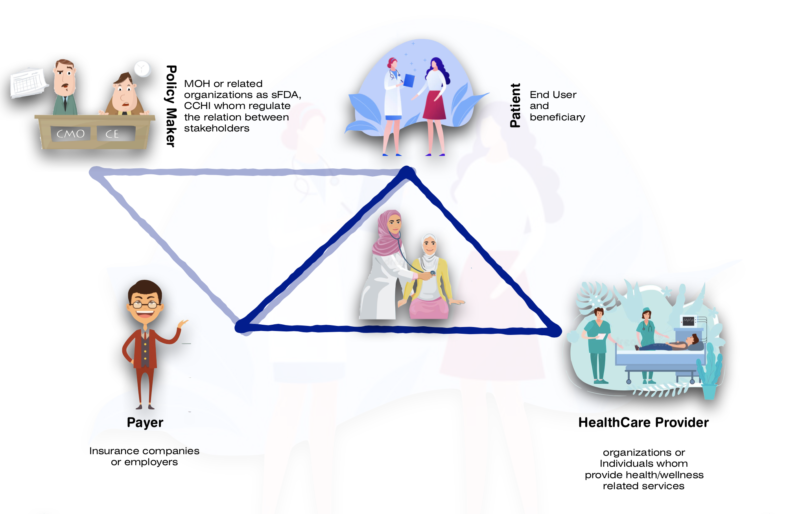
Patients, Healthcare providers, Payers, Employers, Pharmaceuticals, and the Government are the main stakeholders meanwhile the most important stakeholder is the equilibrium between all stakeholders and any initiative for improvement should keep eye on the reflection on each stakeholder side and how can you keep the equilibrium between them.
At the center of the health care system is the patient. The patient is seeking to improve or maintain their health, from the providers of health care services. The patient also is financing some portion of their health care, through the payment of premiums, taxes, and any out-of-pocket expenses.
Health care providers include physicians and nurses, Health care is paid for by a variety of sources including employers that fund health insurance for their employees and their dependents. Elderly, disabled, and low-income individuals, receive insurance coverage that is funded by state and federal governments.
In most instances, an insurance company is involved in the health care transaction, acting as a risk pooling entity or third-party administrator for the employer or government purchaser.
Insurance companies pay for health care services with the funds they receive as premium dollars. Government purchasers pay for health care services with the funds they receive as tax revenue. The pharmaceutical industry develops new drugs, test them for efficacy and safety, and promotes them for use by doctors. To help contextualize this a bit,
Which Payment model could enhance the Healthcare ecosystem in terms of $ savings, health improvement, productivity improvement, and/or deceleration in the rate of annual cost increases?
ACO | Accountable care organization with a bundled payment model.
One of the biggest reasons cited for these deficiencies is the fee-for-service payment model.
In order for healthcare delivery to transform, payment models need to evolve to ensure that providers are paid for providing the right care, at the right time, in the right setting
Why
1. The system is broken and is not sufficiently coordinated, so it produces less than optimal results. the patient is most affected by these inefficiencies and less than optimal health care delivery.
2. Profit before value. The current health care delivery system is structured in response to that payment model, which pays providers for the volume and intensity of services provided.
3. Positive Impact on Value and trend Healthcare trend is a function of changes in:
3.1 Utilization, Unit cost,
reduced high-cost acute services like hospitalizations, emergency room visits, specialty visits, and procedures that are offset by higher costs for primary care.
3.2 Severity,
Patient compliance will be improved, and this will may prevent some complications like diabetic foot ulcers or peripheral neuropathy for diabetic patient
3.3 Provider mix.
PCP will have a bigger role in the healthcare ecosystem.
Do we have a real need/example to prove the concept?
All activities till now are under observation but in the COVID-19 case, we found that unnecessary visits to hospitals were decreased and finical equilibrium between stakeholders was affected. Insurance companies’ margins improved, Providers were negatively affected, and care become difficult to be delivered for some patients. And the offering of telemedicine and distance medicine concepts had raised and market pushed this need to keep the equilibrium. This metaphor we can build on
What are the potential unintended consequences and ways that you propose to mitigate the risks from occurring?
There may also be higher costs for prescription drugs and labs, as patients are more compliant with their medications and monitoring of their conditions.
Improved productivity is more difficult to quantify
For risk mitigation: –
2 sides risk can be overcome by
1. integration and saving sharing in the fairway between delignated stakeholders
2. revisit the revenue centers’ contributions on the providers’ side (medication will be increased, and admission will be decreased)
Conclusion
Treating a patient not just a disease is not an easy mission and the sustainability of the healthcare ecosystem needs more effort to offer the right value to the right customer at the right time from the right HCPs. An ACO is a great start.



